Bedside assessment of left atrial pressure in critical care: A multifaceted gem
Web link: Open online
Zotero link: Open in Zotero
Tags: Echocardiography, haemodynamics,
Abstract
Evaluating left atrial pressure (LAP) solely from the left ventricular preload perspective is a restrained approach. Accurate assessment of LAP is particularly relevant when pulmonary congestion and/or right heart dysfunction are present since it is the pressure most closely related to pulmonary venous pressure and thus pulmonary haemodynamic load. Amalgamation of LAP measurement into assessment of the ‘transpulmonary circuit’ may have a particular role in differentiating cardiac failure phenotypes in critical care. Most of the literature in this area involves cardiology patients, and gaps of knowledge in application to the bedside of the critically ill patient remain significant. Explored in this review is an overview of left atrial physiology, invasive and non-invasive methods of LAP measurement and their potential clinical application.
Notes
Annotations
(9/11/2022, 5:53:55 PM)
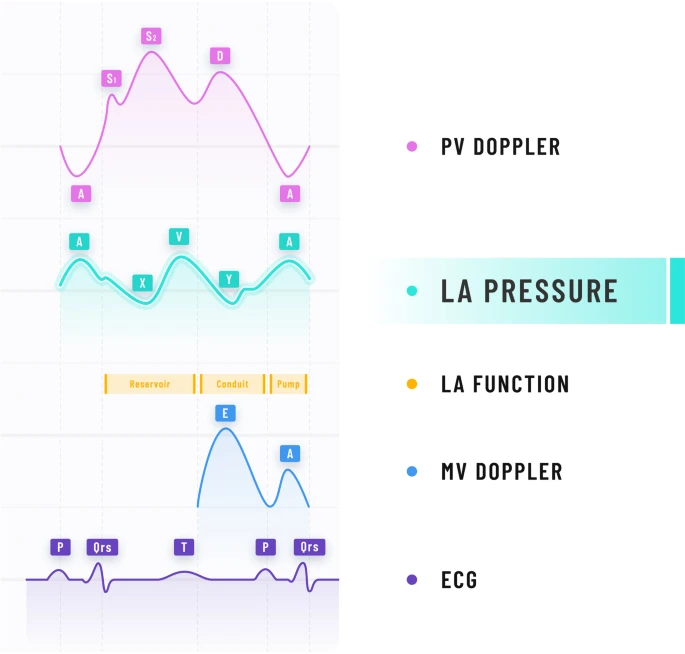
“the left atrium is a key component of the ‘transpulmonary circuit’ with upstream and downstream functions as
- reservoir,
- conduit and
- pump” Go to annotation (Bowcock and Mclean, 2022, p. 2)
“Mean LAP and LVEDP are not telling us the same thing yet are often used interchangeably. The LVEDP provides information about the LV operating compliance and is the closest estimate of LV preload as a surrogate for LVEDV. Patients with similar LVEDP can have markedly different LAP, which is determined by the operating compliance of the LA” Go to annotation (Bowcock and Mclean, 2022, p. 4)
“The mean LAP integrates the atrial pressure tracing throughout systole and diastole providing a measure of the hemodynamic load determined by the LA operating compliance (and indirectly left ventricular operating compliance through atrioventricular coupling)” Go to annotation (Bowcock and Mclean, 2022, p. 4)
“It is the mean LAP that is reflected back to the pulmonary venous circulation impacting right ventricular performance” Go to annotation (Bowcock and Mclean, 2022, p. 4)
“Mid A‐wave amplitude) is recommended in consensus statements to estimate end-diastolic LAP that correlates most closely with LVEDP [11], whereas the mean LAP is obtained by temporal integration of the instantaneous PAOP over the entire cardiac cycle” Go to annotation (Bowcock and Mclean, 2022, p. 4)
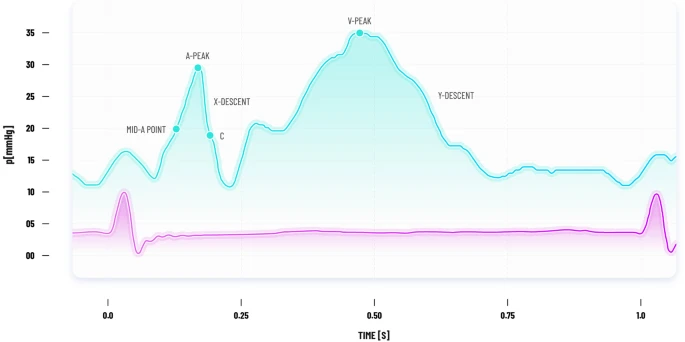
“Mean LAP and end-diastolic LAP can differ significantly in the presence of large ‘V’ waves that occur in severe mitral regurgitation and with reduced LA compliance” Go to annotation (Bowcock and Mclean, 2022, p. 4)
“Valvular disease (Mitral valve stenosis and regurgitation (meanLAP > LVEDP), Aortic regurgitation (meanLAP < LVEDP))” Go to annotation (Bowcock and Mclean, 2022, p. 5)
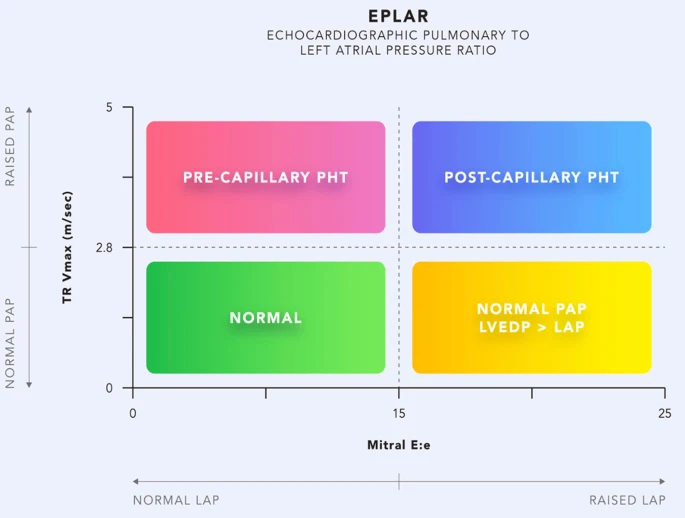
“isolated post-capillary PH may derive benefit from diuretics, and pulmonary vasodilators in this group may worsen pulmonary oedema” Go to annotation (Bowcock and Mclean, 2022, p. 10)
“A septal E/e′ of > 11, as well as lack of mitral E velocity beat to beat variation, are suggestive of raised LAP in AF” Go to annotation (Bowcock and Mclean, 2022, p. 11)
“Although a normal E/e′ does not rule out high LAP, an E/e′ > 15 does have a high specificity in identifying a high LAP” Go to annotation (Bowcock and Mclean, 2022, p. 11)
“At the other extreme, a low lateral E/e′ of < 8 has shown good diagnostic accuracy to predict PAOP < 18 mmHg” Go to annotation (Bowcock and Mclean, 2022, p. 11)
“A non-invasive, rapid beside screening tool to identify patients with possible raised LAP could be ‘the rule of 8’s’: lateral E/e′ > 8 [34] and a lateral e’ ≤ 8 cm/s [32]. This tool could serve as a trigger to temporarily ha” Go to annotation (Bowcock and Mclean, 2022, p. 11)
“LA strain should be measured using a non-foreshortened apical-4-chamber (A4C) view of the LA where values of LA strain for reservoir, conduit and pump functions are measured” Go to annotation (Bowcock and Mclean, 2022, p. 11)
“LA strain didn’t perform well in predicting LVFP in those with AF.” Go to annotation (Bowcock and Mclean, 2022, p. 12)
“An important concept to appreciate is that the ‘diastolic stress test’ of critical illness can shift patients from a normal ‘resting’ LAP to a high LAP state, with corresponding increases in E/e′ ratio. This is because the mitral annular velocity (e’) of the stiff left ventricle cannot increase to match the increased mitral E velocity as occurs with increased cardiac output demand [27]. This can be particularly problematic during ventilatory weaning leading to Weaning-induced Pulmonary Oedema (WiPO)” Go to annotation (Bowcock and Mclean, 2022, p. 12)
“A PAOP ≥ 18 mmHg was a commonly accepted criterion to define cardiogenic oedema in ARDS [52]. However, it was not a ‘hard’ value, was seldom measured and it was increasingly appreciated that raised LVFP could coexist with ARDS, hence it was removed from revised diagnostic criteria” Go to annotation (Bowcock and Mclean, 2022, p. 13)