During Med Residency In...
Highlights
- During med residency in late 1990s, I noticed that patients w/ hypermobile joints ("double jointed") frequently had episodes of unexplained tachycardia, headache/lightheadedness. (View Tweet)
- I suspected Marfan's but never found the classic signs for it (i.e., tall stature, high arched palate, or "thumb sign" [see images below from https://t.co/8fHBCq2FTw ]).
Plus, for whatever reason, many of these patients were women.
 (View Tweet)
(View Tweet)
- So I chalked this to some unknown connective tissue disorder which may/may not have some relationship with these symptoms.
Years later, I found out that these patients likely had Ehler-Danlos syndrome #EDS. (Yes, I should have known, but my Harrison's textbook was no UptoDate). (View Tweet)
- Even more recently, I found out that many EDS patients suffer from #dysautonomia (specifically, #POTS).
In a recent retrospective analyses of 98 EDS patients, nearly 80% had dysautonomia presenting w/ palpitations, dizziness and syncope.

 (View Tweet)
(View Tweet)
- 1.) Lower extremity have highly distensible vasculature that lead to low PVR (arteries/arterioles) and pooling of blood (veins) upon standing. The reduced venous return does not necessarily lead to hypotension, but sympathetics NS compensation leads to tachycardia/palpitations. (View Tweet)
- 2.) Baroreceptors in carotid/aortic bodies are located in the tunica adventitia of vessel, amidst loose connective. The highly compliant connective tissue do not generate high wall stresses so baroreceptors are not activated even during systole. (View Tweet)
- Baroreceptors thus chronically sense low pressure and hence activate the SNS.
This explains why EDS patients were found (via autonomic tests) to have "resting sympathetic overactivity but decreased sympathetic reactivity to stimuli".
Of note, Parasympathetic NS remained intact.
 (View Tweet)
(View Tweet)
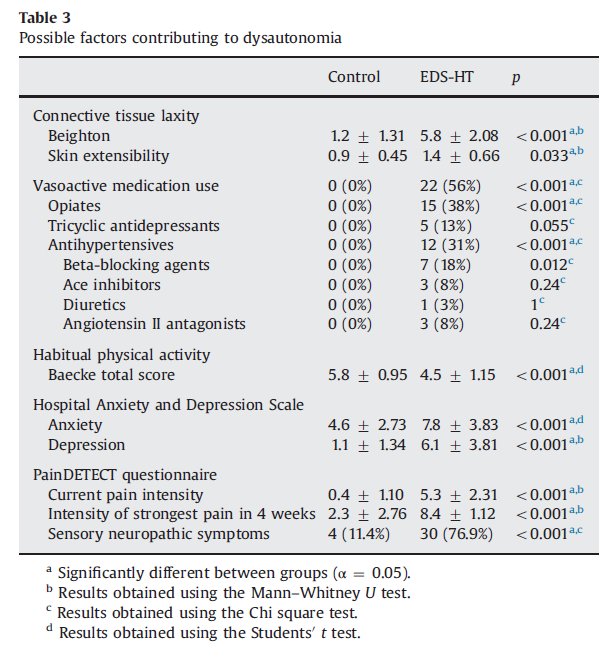
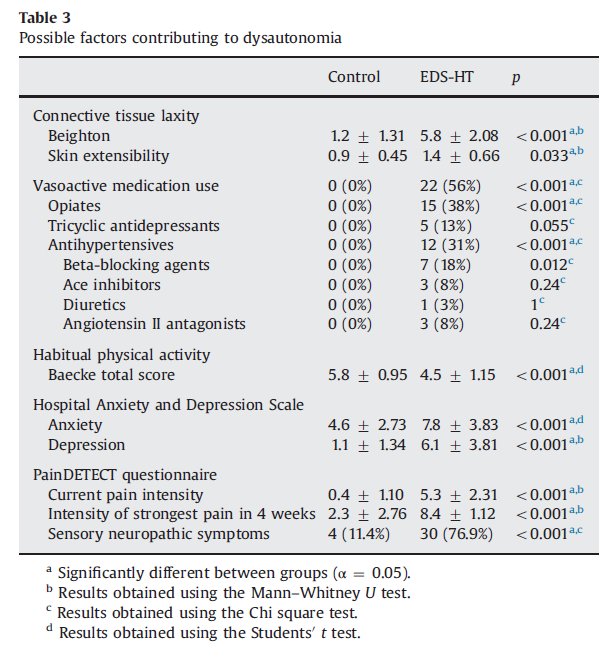
- 3.) Use of vasoactive medications (like opiates, trazodone, antihypertensives, TCA, etc) in this population may also contribute to dysautonomia - but I would probably guess it plays a minor role.
Figure from https://t.co/32uOAe0Fnv
 (View Tweet)
(View Tweet)
- From this same publication, it was evident that level of distensibility was quite important:
".... we found that parameters reflecting collagen laxity, such as skin extensibility and the Beighton score, were related to parameters of vasodilatation .. and to increased HR... (View Tweet)
- ... Moreover, in the linear regression analysis, skin extensibility was identified as the most important predictor for the severity of sympathetic dysfunction, stronger than vasoactive medication use." (View Tweet)
- These autonomic NS symptoms are not trivial and can be debilitating.
In 2019, Ms. Nicola Blackwood - a prominent member of the UK parliament then - passed out during a congressional session. She has made her EDS and POTS diagnosis quite public.
https://t.co/H7KSp0KSPR (View Tweet)
- Ultimately, autonomic dysfunction in hEDS is very common and greatly underappreciated. Surprisingly little is known about the underlying mechanism. There is a lot more to connective tissue physiology than we know. Keep an eye on this space.
End/ (View Tweet)
During Med Residency In...
Highlights
- During med residency in late 1990s, I noticed that patients w/ hypermobile joints ("double jointed") frequently had episodes of unexplained tachycardia, headache/lightheadedness. (View Tweet)
- I suspected Marfan's but never found the classic signs for it (i.e., tall stature, high arched palate, or "thumb sign" [see images below from https://t.co/8fHBCq2FTw ]).
Plus, for whatever reason, many of these patients were women.
 (View Tweet)
(View Tweet)
- Even more recently, I found out that many EDS patients suffer from #dysautonomia (specifically, #POTS).
In a recent retrospective analyses of 98 EDS patients, nearly 80% had dysautonomia presenting w/ palpitations, dizziness and syncope.

 (View Tweet)
(View Tweet)
- 1.) Lower extremity have highly distensible vasculature that lead to low PVR (arteries/arterioles) and pooling of blood (veins) upon standing. The reduced venous return does not necessarily lead to hypotension, but sympathetics NS compensation leads to tachycardia/palpitations. (View Tweet)
- 2.) Baroreceptors in carotid/aortic bodies are located in the tunica adventitia of vessel, amidst loose connective. The highly compliant connective tissue do not generate high wall stresses so baroreceptors are not activated even during systole. (View Tweet)
- Baroreceptors thus chronically sense low pressure and hence activate the SNS.
This explains why EDS patients were found (via autonomic tests) to have "resting sympathetic overactivity but decreased sympathetic reactivity to stimuli".
Of note, Parasympathetic NS remained intact.
 (View Tweet)
(View Tweet)
- 3.) Use of vasoactive medications (like opiates, trazodone, antihypertensives, TCA, etc) in this population may also contribute to dysautonomia - but I would probably guess it plays a minor role.
Figure from https://t.co/32uOAe0Fnv
 (View Tweet)
(View Tweet)
- From this same publication, it was evident that level of distensibility was quite important:
".... we found that parameters reflecting collagen laxity, such as skin extensibility and the Beighton score, were related to parameters of vasodilatation .. and to increased HR... (View Tweet)
- ... Moreover, in the linear regression analysis, skin extensibility was identified as the most important predictor for the severity of sympathetic dysfunction, stronger than vasoactive medication use." (View Tweet)
- Ultimately, autonomic dysfunction in hEDS is very common and greatly underappreciated. Surprisingly little is known about the underlying mechanism. There is a lot more to connective tissue physiology than we know. Keep an eye on this space.
End/ (View Tweet)
 (View Tweet)
(View Tweet)
 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)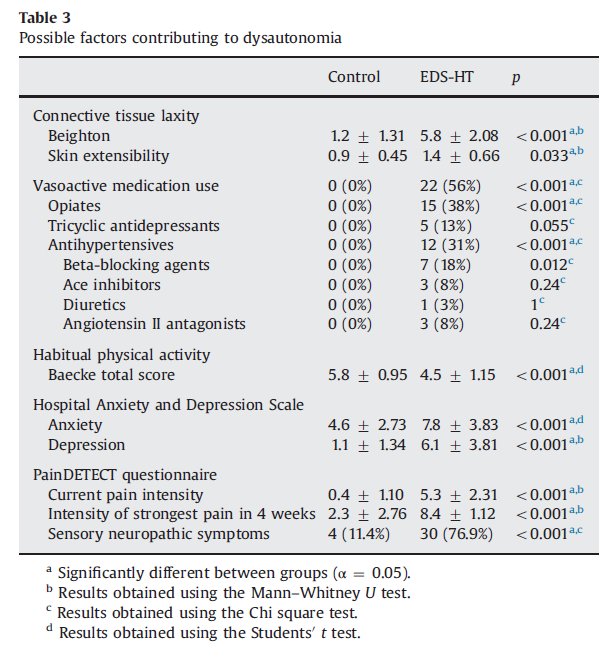 (View Tweet)
(View Tweet)
 (View Tweet)
(View Tweet)
 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)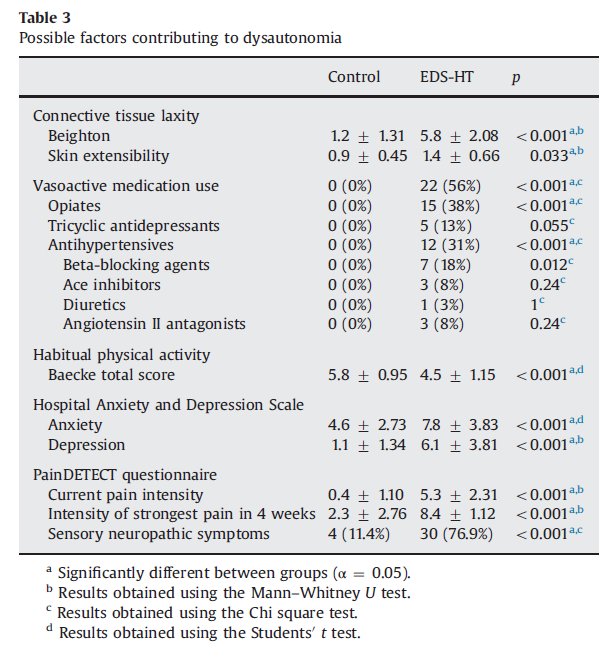 (View Tweet)
(View Tweet)