As a Nephrologist, Why D...
Highlights
- As a Nephrologist, why do I love vasopressin? Particularly when I see patients in the CCU?
My ode to vasopressin in a 🧵
#medtwitter #cardstwitter #nephtwitter @MedTweetorials (View Tweet)
- Right off the bat let's acknowledge that the following trials show no mortality benefit in critically ill patients with vasopressin. But that's not the point - we only care about the kidneys right now because I'm a Nephrologist. (View Tweet)
- Before we get to hearts we need to borrow from the sepsis literature.
First a small study from 2002
💥24 pts w/septic shock
💥vasopressin v norepinephrine x4 hrs, titrated to BP
💥Vasopressin group = better UOP and CrCl
https://t.co/iYoRq9Q80h

 (View Tweet)
(View Tweet)
- Lauzier et al from 2006
💥23 pts w/septic shock
💥Vasopressin v NE. Equal BPs at 48 hrs, however NE required in 36% of vaso patients to do so
💥Better CrCl in the vasopressin group
https://t.co/ThCDmOOUg0
 (View Tweet)
(View Tweet)
- Morelli et al 2009
💥45 pts w/septic shock
💥terlipressin v vasopressin v norepinephrine
💥Again worse kidney function, by creatinine criteria, in the norepinephrine group
https://t.co/R4AeShXLay
 (View Tweet)
(View Tweet)
- In 2008 in the NEJM we got the VASST trial. 778 pts w/septic shock randomized to vasopressin or NE. No difference in mortality.
BUT: Gordon et al performed a post-hoc analysis and found that "at risk pts" (creatinine x1.5) had lower rates of progression of AKI with vasopressin
 (View Tweet)
(View Tweet)
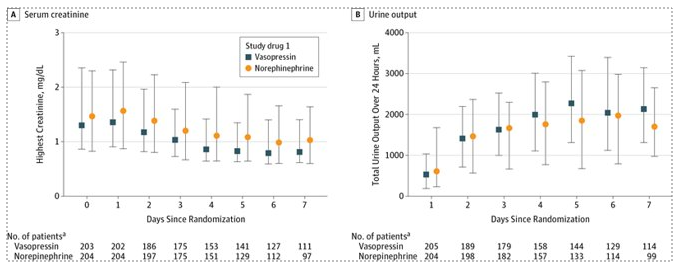
- Same group published the VANISH trial in JAMA in 2016.
💥409 pts w/septic shock
💥vasopressin v NE (2x2 design with steroid arms as well)
💥NO difference in kidney-failure free days between groups
🔥BUT better UOP and decreased use KRT in the vaso group
https://t.co/70e8CkAmlg
 (View Tweet)
(View Tweet)
- How about vaso post Cardiac Surgery? Enter the VANCS trial from 2017.
💥330 pts with vasoplegic shock (MAP<65 and CI>2.2 resistant to fluids)
💥vaso vs NE
💥Again, better kidney function in the vaso group
https://t.co/wIzBhDgpJW
 (View Tweet)
(View Tweet)
- OK, so there's seems to be evidence to suggest that vasopressin improves kidney outcomes. But how do we extrapolate to the CCU?
💡In low flow states, RBF falls well before GFR due to the kidney's ability to autoregulate
🔥Primary mechanism for this is efferent vasoconstriction
 (View Tweet)
(View Tweet)
- Borrowing from HRS. Relationship b/w RBF and BP is altered during SNS activation (which happens with CRS as well) - with a rightward shift in the renal autoregulatory curve so RBC is critically dependent on BP.
🔥Concept here is RPP (MAP-CVP) and should be considered in all pts (View Tweet)
- 💥While NE constricts both efferent/afferent arterioles - vasopressin appears to exert a preferential effect on the efferent arteriole, which may explain the beneficial kidney outcomes
We use this to our advantage in certain cases of diuretic resistance
https://t.co/3Jkra9gq5m

 (View Tweet)
(View Tweet)
- This may be particularly useful in pts with right heart failure since you're not as concerned about afterload with a presumably functioning LV.
💥Vaso does not appear to impact the pulm artery, whereas NE exerts a vasoconstrictive effect
https://t.co/q8Hir6R0AG
 (View Tweet)
(View Tweet)
- Conclusions:
💥Vasopressin assoc with better kidney outcomes in critically ill pts
💥Preferential efferent vasoconstriction may explain the above. Can use this in certain cases of DR
💥RPP (MAP-CVP) should be considered in all pts
💥May be particularly useful in RV failure
END. (View Tweet)

 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)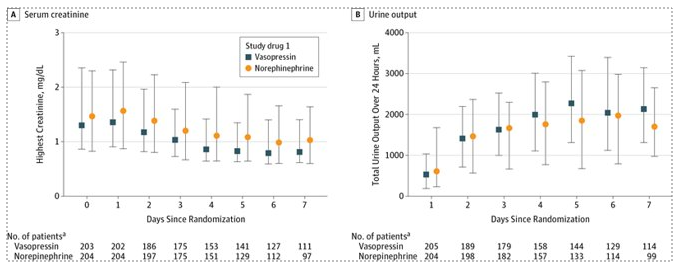
 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)
 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)